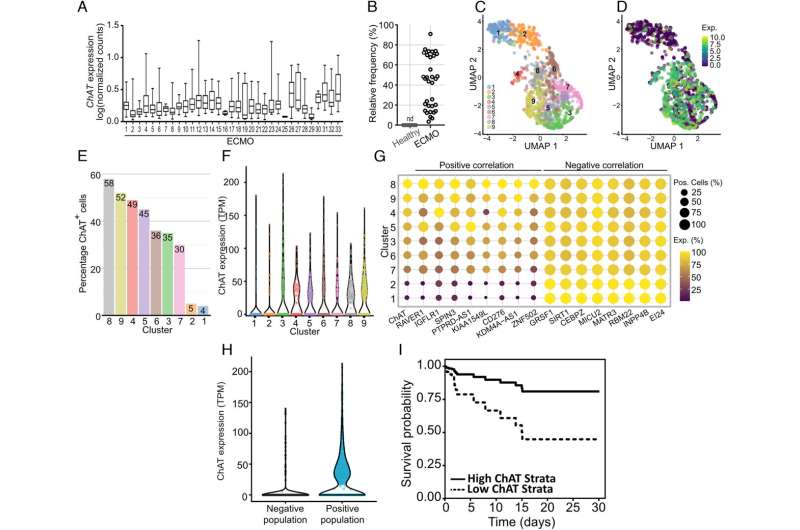
Acetylcholine regulates blood flow, but the source of blood acetylcholine has been unclear. Now, researchers at Karolinska Institutet have discovered that certain T cells in human blood can produce acetylcholine, which may help regulate blood pressure and inflammation. The study, which is published in PNAS, also demonstrates a possible association between these immune cells in seriously ill patients and the risk of death.
Continue reading “Study discovers T cells in human blood secrete a substance that affects blood pressure and inflammation”Category: Inflammation and Your Organs
Gout Comes With Increased Heart Risk
Incident gout and risk of first-time acute coronary syndrome: a prospective, population-based, cohort study in Sweden
Panagiota Drivelegka MD, PhD,Lennart T.H. Jacobsson MD,Ulf Lindström MD,Karin Bengtsson MD, PhD,Mats Dehlin MD
First published: 12 September 2022
https://doi.org/10.1002/acr.25018
Abstract
Objective
To investigate the risk of first-time acute coronary syndrome (ACS) in a large cohort of primary and secondary care patients with incident gout, compared to the general population.
Continue reading “Gout Comes With Increased Heart Risk”Sleep and your health
Sleep and your health
As life gets more hectic, it is all too easy to go without sleep. In fact, many Americans only get 6 hours of sleep a night or less.
You need ample sleep to help restore your brain and body. Not getting enough sleep can be bad for your health in a number of ways.
Why you Need Sleep
Sleep gives your body and brain time to recover from the stresses of the day. After a good night’s sleep, you perform better and are better at making decisions. Sleep can help you feel more alert, optimistic, and get along with people better. Sleep also helps your body ward off disease.
Continue reading “Sleep and your health”Diuretics and Gout: Is there a connection?
High Blood Pressure, Prescription Diuretics, and Gout
What is high blood pressure?
High Blood Pressure, also called hypertension, is when blood puts too much pressure against the walls of your arteries. About 1 in 3 adults have high blood pressure, usually with no symptoms. But it can cause serious problems such as stroke, heart failure, heart attack, and kidney disease.
What lifestyle changes can help lower high blood pressure?
Continue reading “Diuretics and Gout: Is there a connection?”Stress accelerates immune aging, study finds
Traumatic life events, discrimination prematurely weaken body’s mix of immune cells
Date: June 13, 2022
Source: University of Southern California
Summary: Stress — in the form of traumatic events, job strain, everyday stressors and discrimination — accelerates aging of the immune system, potentially increasing a person’s risk of cancer, cardiovascular disease and illness from infections such as COVID-19, according to a new study. The research could help explain disparities in age-related health, including the unequal toll of the pandemic, and identify possible points for intervention.
Continue reading “Stress accelerates immune aging, study finds”Does Gout Increase The Cardiovascular Disease Risk Factor?
Cardiovascular Disease and Gout

The prevalence of cardiovascular disease continues to rise and is among the leading cause of mortality in the world. Inflammatory conditions such as Rheumatoid Arthritis and Gout are often associated with a higher risk and earlier onset of this disease. Research links gout to an increased risk of several types of cardiovascular disease, including heart attack, heart failure, and atrial fibrillation, or an irregular heartbeat. Epidemiological, experimental, and clinical data show that patients with hyperuricemia SUA are at increased risk of cardiac, renal, and vascular damage and CV events. Continue reading “Does Gout Increase The Cardiovascular Disease Risk Factor?”
Gout ‘more than doubles’ risk of kidney failure
Largest ever study on subject uses data from more than 620,000 patients in UK health system
Date: August 28, 2019
Source:University of Limerick
Summary: Patients with gout are at increased risk of chronic kidney disease and kidney failure, according to new research.
Patients with gout are at increased risk of chronic kidney disease and kidney failure, according to new University of Limerick (UL), Ireland led research.
In one of the largest and most detailed studies ever conducted, patients recruited in general practice with a diagnosis of gout were more than twice as likely to develop kidney failure than those without, according to the study led by researchers at University of Limerick’s (UL) Graduate Entry Medical School (GEMS).
Continue reading “Gout ‘more than doubles’ risk of kidney failure”Wearable sweat sensor detects gout-causing compounds
Date:November 25, 2019
Source: California Institute of Technology
Summary: Scientists have developed an easier way to mass-produce highly sensitive sweat sensors that can detect a variety of low-concentration compounds related to health conditions.
There are numerous things to dislike about going to the doctor: Paying a copay, sitting in the waiting room, out-of-date magazines, sick people coughing without covering their mouths. For many, though, the worst thing about a doctor’s visit is getting stuck with a needle. Blood tests are a tried-and-true way of evaluating what is going on with your body, but the discomfort is unavoidable. Or maybe not, say Caltech scientists.
Continue reading “Wearable sweat sensor detects gout-causing compounds”Is Uric Acid Good or Bad?
Purines perform multiple important functions within our cells, including regulating energy metabolism and signaling the energy conversion from one to another. Purines are essentially the building blocks for all living things as a necessity for the growth, proliferation and survival of all cells. The two purine bases, adenine and guanine, create bonds that form the DNA ladder. Humans breakdown purines and convert them into uric acid.
Uric acid happens to be a potent DNA protector. All other mammals possess an enzyme known as uricase. Uricase converts uric acid into allantoin, which can easily travel through the bloodstream and readily eliminated through the urine. Humans do not possess this enzyme, therefore, we cannot oxidize uric acid into the more soluble compound of allantoin. Our liver and kidneys are left to do the all-important jobs of purine breakdown and uric acid disposal, conducted respectively.
Blood serum uric acid levels are determined by two components:
- uric acid synthesis
- uric acid excretion
Synthesis takes place in the liver as a result of the breakdown of purines. Purine levels are mostly determined by what is naturally produced by the body, with approximately the other 30% absorbed from the food we eat. The second component, uric acid excretion, is determined by the rate at which the kidneys are able dispose of the excess. According to a study conducted by Hyon K. Choi in 2005, about 90% of hyperuricemia is attributed to impaired renal excretion.
As we mentioned above, uric acid is a potent antioxidant and DNA protector. Could this be why only 10% of the uric acid that enters a normal human kidney is disposed of? Would it be safe to assume the other 90% that is reclaimed and sent back into the bloodstream is done so for our bodies to utilize its powerful antioxidant and free radical neutralizing powers?
According to science…..
Uric acid is responsible for the neutralization of over 50% of the free radicals in our bloodstream. Considering humans and primates are unable to naturally produce Vitamin C, we may have inherited the ability to utilize uric acid. Uric acid remains extremely controversial and difficult to manage. On one hand, uric acid protects high-oxygen tissues (like the brain) from damage and has been shown to increase the risks of several neurological disorders in the presence of sub-par levels. On the other hand, high-serum uric acid levels are inversely associated with the severity of several diseases, especially the state of cardiovascular diseases.
Is there a balance?
Yes, although the course(s) of action to achieve this balance may be equally as complex, as well as individually determined. As a former Gout sufferer, I naturally ventured down the path of reducing my purine intake by focusing on my diet. Once I understood a bit more about the roles of purines and uric acid I was able to conclude that this path was not going lead me to success.
I asked myself the following questions:
- If only 30% of the purines in my body come directly from food, then will a low-purine diet do anything to help with the main 70% of my production?
- Do I have any control over the other 70% that occurs naturally in my body?
- Am I doing anything to directly contribute to higher purine production aside from the food I eat?
- If the food I eat is low-purine, but still unhealthy, does that have any impact on the amount my body is naturally producing?
The last question truly gave me pause. If the natural purine production stems from normal DNA and RNA turnover, were there things I was doing to my body to cause my cells to die and turnover faster than usual?
This brought me to another series of questions, ones I believe to be more relevant to my cause:
- Do my medications and over-the-counter drugs contributing to faster cell death?
- Was I hydrated enough? Cellular dehydration is extremely common and definitely causes cellular turnover.
- Did my slightly overweight body and lack of exercise have anything to do with the health of my cells?
- Was my rather heavy alcohol consumption a bigger problem than just the purines alone? Does it affect my cells, too?
- Did my high stress life contribute to faster cellular death?
- Does my sweet tooth and sugar intake affect my cells and uric acid production?
- If my body can’t naturally produce certain vitamins and antioxidants, could I help my body by supplying enough in my diet and supplementation in hopes of my kidneys not reclaiming as much uric acid to help in their absence?
Looking ahead….
These are some really important questions that opened my eyes to a whole new approach and a whole new outlook on the importance of taking better care of myself. These questions initially targeted my efforts to gauge my cellular health (or lack thereof), but also really put my kidney and liver health into question. Many of us unknowingly damage the health of our cells, furthering excess uric acid production. In doing so, we are also placing unnecessary strain on the very organs we need to help us rid of the excess uric acid. What a conundrum!
These epiphanies led me to better health, elimination of my medications (blood pressure, cholesterol, and Gout), correction of my glucose levels, secured my beliefs in the right all natural remedies, led to my blog, and changed my life! It doesn’t have to be so overwhelming. Take a step back and look at the bigger picture and you will find there is a lot of common sense in play here, and even more common sense solutions. Take it slow, one adjustment at a time for attainable goals. This site offers a series of articles to highlight a bit more on the specifics regarding stress, hydration, diet, and much more
Here’s to your Gout and Inflammation free 2020 and beyond!
Gout and Kidney Disease
Chronic kidney disease (CKD)
Chronic kidney disease (CKD) limits the amount of waste filtration your body is capable of processing. Uric acid is not seen as a foreign matter to the body, therefore is usually last to be dealt with from a toxin filtering standpoint. This can allow for uric acid build-up, and, in turn, the increased likelihood of developing Gout. The medications used to treat kidney disease have also been associated with drug-induced cases of Gout. Diuretics and beta blockers are typically used for kidney disease induced high blood pressure and are well known to contribute to Gout development.
There is enough scientific research to confirm that kidney disease can cause Gout. How about the opposite? Can Gout lead to kidney disease? The chicken or the egg? Uric acid is filtered through the kidneys, an undeniable relation to both diseases. While this connection may be less established, the evidence is certainly present. Each condition is well-equipped to feed the other.
Continue reading “Gout and Kidney Disease”